Introduction
Have you been dealing with persistent bloating, discomfort and frustrating digestive issues that won’t go away even after treatment? Small Intestinal Bacterial Overgrowth (SIBO) is challenging enough, but biofilms—protective layers created by bacteria— can make it even tougher to manage. These biofilms allow bacteria to hide from treatments, which could explain why SIBO often recurs despite your multiple attempts to resolve it. In this post, we’ll explore the connection between biofilms and SIBO, why biofilms matter, and what you can do to get rid of them once and for all.
What Are Biofilms?
A biofilm is basically a group of microbes like bacteria, funghi and algae that stick to a surface and to each other. They are surround themselves by a protective, glue-like substance called an extracellular polymeric matrix (1) or in other words the microbes are together in a sort of shield like structure surrounded by sticky substances. Why do microbes form biofilms? Simply put, it’s their way of protecting themselves from anything that might try to disrupt their plans, like: antibiotics, antimicrobials, and the body’s immune system.
Acoording to science, biofilm are related to around 80% of human bacterial infections (3). That’s worrying, because these infections can be incredibly hard to treat because biofilms create a protective barrier that shields the bacteria from treatments like antibiotics and the immune system, making the bacteria hiding in this biofilm antibiotics-resistant (2).
How Do They Relate to SIBO?
If you’re dealing with SIBO, SIFO, candida, H. pylori, or other gut issues, biofilms are often part of the problem. Ignoring them can make it almost impossible to fully tackle these conditions. It is one of the reasons why relapse is a common challenge in SIBO patients. One study showed that 45% of their patients had a relapse of SIBO after antibiotics and 43.7% relapsed within 9 months (4)!
Biofilms may contribute to both chronic and recurring symptoms by:
-
- Protecting bacterial colonies in the small intestine: these bacteria can survive treatments that normally eliminate free-flowing bacteria.
- Preventing antibiotics and herbal treatments from fully getting rid of the bacteria, making it easy for them to come back.
- Contributing to inflammation and damaging the gut lining.
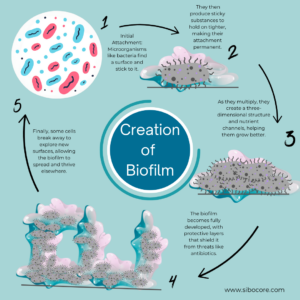
How Are Biofilms Formed?
Biofilm formation happens in five main stages (2), and it’s actually a pretty clever process. Let’s break it down:
-
The Initial Attachment (Reversible)
At first, bacteria are floating around freely (planktonic bacteria) and eventually bump into a surface. At this stage, their attachment is still temporary—they can decide to stick around or move on if the environment isn’t quite right. -
The Commitment (Irreversible Attachment)
Once the bacteria decide they like the surface, they commit. They start laying down the extracellular matrix consisting of a mix of sugars, proteins, DNA, and cell debris. It’s like the bacteria’s armor against outside threats. -
Building a Community (Microcolony Formation)
Now, the bacteria get busy multiplying and forming tiny clusters called microcolonies. At this point, they’re fully attached, and there’s no turning back—the attachment is now permanent. -
The Growth Phase (Maturation)
This is where things get serious. The biofilm grows into a full-blown, three-dimensional structure with layers of bacteria, all protected by their sturdy matrix. -
Spreading Out (Dispersion)
Once the biofilm is mature, some bacteria decide it’s time to move on. They break free and become planktonic again, floating away to find a new surface where they can do it all again.
Causes of Biofilm Formation in SIBO
Biofilms don’t appear overnight. They develop under specific conditions that allow bacteria to thrive. There’s usually 4 key reasons for bacteria to form biofilms: defense, colonization, community and default growth mode (5).
- Colonization: Bacteria anchor themselves in good t nutrient-rich areas, ensuring a steady food supply.
- Defense: Biofilms protect bacteria from harmful conditions within the host, such as immune responses or antibiotics.
- Community: Biofilms enable bacteria to work together and share resources, providing cooperative benefits that help the entire group to live.
- Default Growth Mode: Some researchers suggest that biofilms might be the bacteria’s natural way of growing, with free-floating (planktonic) bacteria being more of a laboratory phenomenon.
Most of the reasons in SIBO, are related to the colonization, as they in one way or another help to create or foster a nutrient rich environment:
- Dietary Habits: Bacteria really love to eat any type of sugar, meaning that people with diets high in sugar and refined carbohydrates can stimulate bacterial growth in their guts (6). On top of that, insufficient fiber reduces the production of short-chain fatty acids, which support gut health (7).
- Gut Motility Issues: Slow movement of food through the small intestine allows bacteria to remain in one place, contributing to biofilm development.
- Previous Antibiotic Use: Antibiotics can disrupt the balance of gut flora, enabling harmful bacteria to dominate and form biofilms.
- Underlying Health Conditions: Disorders like Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD), and diabetes can make these bacterial imbalances worse and therefore promote biofilm growth.
- Chronic Inflammation: Ongoing gut inflammation creates an environment conducive to biofilm formation, because it can also damage the gut lining.

Symptoms of SIBO Associated with Biofilms
The symptoms of SIBO caused by biofilms are often similar to traditional SIBO symptoms, but they tend to be more persistent and harder to treat.
-
- Chronic bloating and gas, especially after meals.
- Altered bowel habits, such as diarrhea or constipation (often dependent on which type of SIBO you have).
- Abdominal pain or cramping.
- Persistent fatigue and low energy levels.
- Brain fog: Difficulty concentrating or feeling mentally sluggish, some even describe it as a feeling of being ‘not completely there’ or ‘drunk’.
- Nutrient deficiencies, including vitamin B12, iron, and fat-soluble vitamins.
- Symptoms frequently recur after treatment.
- Increased sensitivity to foods, especially fermentable carbohydrates.
Diagnosing Biofilm-Related SIBO
Diagnosing SIBO with biofilms can be challenging, as traditional SIBO testing methods do not capture biofilms in anyway. Next to that, they may hide bacteria, leading to false negatives. Also, other gut disorders may have similar or overlapping symptoms. This can make it a lot harder to find out what it is that you have. I would recommend to get help from a specialized (functional) doctor.
SIBO is usually tested by use of a breath test, which measures the hydrogen or methane levels produced by the bacteria that cause SIBO. There are some other tests that can be done, like a stool test to understand the level of bacteria in your colon and vitamin deficiencies if you have those.
Strategies for Breaking Down Biofilms and Treating SIBO
To deal with SIBO successfully, especially when you also have biofilms, requires you to use different approaches at the same time. Breaking down biofilms is a critical first step to allow antimicrobials or antibiotics to reach the bacteria.
You can use combinations of biofilm disruptors, antibiotics or antimicrobials to treat SIBO and pre- & probiotics to rebalance your gut after treatment.
Step 1: Biofilm Disruptors:
-
- Enzymes like serrapeptase and nattokinase dissolve biofilm layers.
- Herbal antimicrobials, such as berberine, oregano oil, and garlic extract have biofilm-disrupting properties. These can be taken as supplements similarly to antibiotics. Some research even suggests that antimicrobials is just as good as antibiotics in treating SIBO (7).
Dietary Interventions:
SIBO isn’t something you can fix with just diet, and it’s definitely not a quick fix. However, diet can be used to treat symptoms and as an addition to antibiotics or antimicrobials.
-
- Low-FODMAP Diet: Reduces fermentable carbohydrates that feed bacteria.
- Intermittent Fasting: Starves bacteria by depriving them of a continuous food supply.
Step 2: Targeting Bacteria
- Herbal Treatments: Antimicrobials such as oregano oil, cinnamon extract, and neem.
- Antibiotics: Prescription antibiotics like rifaximin or a rifaximin-neomycin combination can target both hydrogen- and methane-producing bacteria
Step 3: Rebalancing the Gut Microbiome
-
Probiotics:
- Restores balance by replenishing beneficial bacteria.
- Strains like Saccharomyces boulardii may prevent biofilm reformation.
-
Postbiotics and Digestive Enzymes:
- Aid in healing the gut lining and improving digestion.
Conclusion:
Biofilms are a significant factor in chronic and recurrent SIBO and one of the reasons why SIBO comes back often. However, we can use targeted treatments that disrupt this bacteria-shield and hopefully get rid of SIBO for good. A well-rounded approach to SIBO, including biofilms is the way to go.
